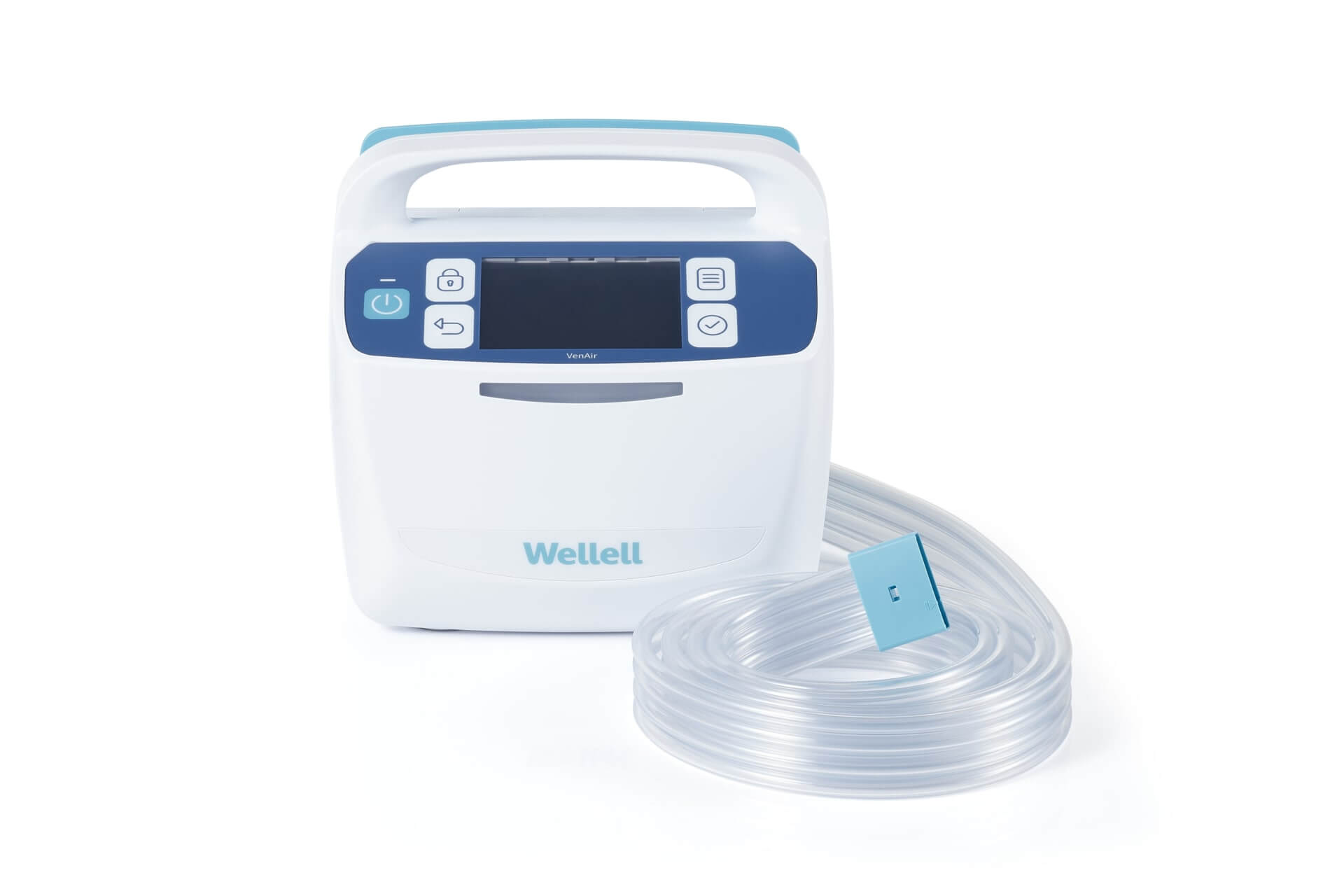
VenAir
Increasing accessibility and personalization for compression care — Decreasing excess length of stay and mortality for inpatient DVT.
Hospitalization causes more than half of VTE cases and excess length of stay and mortality.1 24% is directly related to post-acute complications, requiring up to 10.5 days of in-hospital treatment.2,3
The institutional cost per inpatient DVT event (6-month treatment involving acute care, laboratory, pharmacy, diagnostic, physician fees, hospitalization, and contiguous skilled facility care) ranges from USD 3,906 to over USD 17,168, and an additional USD 264 minimum in hospital costs per day, depending on the severity and patient's health status and age.4
26% readmits within 30-days due to VTE-related complications such as bleeding and post-thrombotic syndrome (PTS)5,6, which can increase costs by 48%.7
Improving inpatient DVT management with automated, portable, comfortable, and intuitive compression therapy reduces the economic burden and readmissions within the first 6 to 12 months and upwards to 10 years after initial diagnosis.8

Automate Compression Delivery
Sensors in the garment detect regional blood circulation levels and instruct the pump to automatically adjust for optimized compression frequency and pressure settings, simplifying the therapy process for healthcare providers and users of all levels.

Reduce Humidity, Improve Comfort
Ambient-adapted design allows VenAir's to efficiently direct and ventilate airflow between the fabric and skin, eliminating humidity, skin irritation, and garment displacement during use, improving user comfort, experience, and therapy outcome.

Deliver Intervention On-The-Road
Built-in battery in the pump powers non-stop compression therapy for up to 6 hours, maintaining therapy continuity and improving treatment outcomes when a reliable power source is not accessible, like during transportation or disasters.

Patented User-First Garment Design
VenAir’s range of patented compression garments (for the thigh, cuff, and foot) conform intimately and comfortably to the skin with zero-creasing and 4 ventilation tubes for optimizing heat reduction, improving ease of use and compression efficacy.

Automate Compression Delivery
Sensors in the garment detect regional blood circulation levels and instruct the pump to automatically adjust for optimized compression frequency and pressure settings, simplifying the therapy process for healthcare providers and users of all levels.

Reduce Humidity, Improve Comfort
Ambient-adapted design allows VenAir's to efficiently direct and ventilate airflow between the fabric and skin, eliminating humidity, skin irritation, and garment displacement during use, improving user comfort, experience, and therapy outcome.

Deliver Intervention On-The-Road
Built-in battery in the pump powers non-stop compression therapy for up to 6 hours, maintaining therapy continuity and improving treatment outcomes when a reliable power source is not accessible, like during transportation or disasters.

Patented User-First Garment Design
VenAir’s range of patented compression garments (for the thigh, cuff, and foot) conform intimately and comfortably to the skin with zero-creasing and 4 ventilation tubes for optimizing heat reduction, improving ease of use and compression efficacy.

Reduce risk of pulmonary embolism, reduce mortality.
15% to 35% of DVT cases turn into pulmonary embolism (PE) and has a high mortality rate from 30% to 50%, making it a leading cause of stroke and secondary infection.9 PE can become a chronic illness for 30% of DVT episodes and require long-term care.10
Reference
- Heit, John A et al. “Relative impact of risk factors for deep vein thrombosis and pulmonary embolism: a population-based study.” Archives of internal medicine vol. 162,11 (2002): 1245-8. doi:10.1001/archinte.162.11.1245
- Geerts, William H et al. “Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition).” Chest vol. 133,6 Suppl (2008): 381S-453S. doi:10.1378/chest.08-0656
- Lozano, Francisco et al. “Home versus in-hospital treatment of outpatients with acute deep venous thrombosis of the lower limbs.” Journal of vascular surgery vol. 59,5 (2014): 1362-7.e1. doi:10.1016/j.jvs.2013.11.091
- O'Brien, Judith A, and Jaime J Caro. “Direct medical cost of managing deep vein thrombosis according to the occurrence of complications.” PharmacoEconomics vol. 20,9 (2002): 603-15. doi:10.2165/00019053-200220090-00004
- Knight, Kevin K et al. “Economic and utilization outcomes associated with choice of treatment for venous thromboembolism in hospitalized patients.” Value in health : the journal of the International Society for Pharmacoeconomics and Outcomes Research vol. 8,3 (2005): 191-200. doi:10.1111/j.1524-4733.2005.04026.x
- Ruppert, Andras et al. “Economic burden of venous thromboembolism: a systematic review.” Journal of medical economics vol. 14,1 (2011): 65-74. doi:10.3111/13696998.2010.546465
- Bullano, Michael F et al. “Longitudinal evaluation of health plan cost per venous thromboembolism or bleed event in patients with a prior venous thromboembolism event during hospitalization.” Journal of managed care pharmacy : JMCP vol. 11,8 (2005): 663-73. doi:10.18553/jmcp.2005.11.8.663
- Heit JA, Mohr DN, Silverstein MD, Petterson TM, O'Fallon WM, Melton LJ 3rd. Predictors of recurrence after deep vein thrombosis and pulmonary embolism: a population-based cohort study. Arch Intern Med. 2000 Mar 27;160(6):761-8. doi: 10.1001/archinte.160.6.761. PMID: 10737275.
- Field TS, Hill MD. Prevention of deep vein thrombosis and pulmonary embolism in patients with stroke. Clin Appl Thromb Hemost. 2012 Jan-Feb;18(1):5-19. doi: 10.1177/1076029611412362. Epub 2011 Jul 6. PMID: 21733942.
- "What Is Venous Thromboembolism? | CDC." Centers for Disease Control and Prevention, 10 Feb. 2020, www.cdc.gov/ncbddd/dvt/facts.html.